Boxed Warning
WARNING: EXACERBATIONS OF HEPATITIS B and RISK OF HIV-1 RESISTANCE IF EPIVIR-HBV IS USED IN PATIENTS WITH UNRECOGNIZED OR UNTREATED HIV-1 INFECTION
Severe acute exacerbations of hepatitis B have been reported in patients who have discontinued anti-hepatitis B therapy (including EPIVIR-HBV). Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue anti-hepatitis B therapy. If appropriate, initiation of anti-hepatitis B therapy may be warranted [see Warnings and Precautions (5.1)].
EPIVIR-HBV is not approved for the treatment of human immunodeficiency virus type 1 (HIV-1) infection because the lamivudine dosage in EPIVIR-HBV is subtherapeutic and monotherapy is inappropriate for the treatment of HIV-1 infection. HIV-1 resistance may emerge in chronic hepatitis B-infected patients with unrecognized or untreated HIV-1 infection. HIV counseling and testing should be offered to all patients before beginning treatment with EPIVIR-HBV and periodically during treatment [see Warnings and Precautions (5.2)].
1. Indications and Usage
EPIVIR-HBV is indicated for the treatment of chronic hepatitis B virus (HBV) infection associated with evidence of hepatitis B viral replication and active liver inflammation [see Clinical Studies (14.1, 14.2)].
The following points should be considered when initiating therapy with EPIVIR-HBV:
- Due to high rates of resistance development in treated patients, initiation of treatment with EPIVIR-HBV should only be considered when the use of an alternative antiviral agent with a higher genetic barrier to resistance is not available or appropriate.
- EPIVIR-HBV has not been evaluated in patients co-infected with human immunodeficiency virus (HIV), hepatitis C virus (HCV), or hepatitis delta virus.
- EPIVIR-HBV has not been evaluated in liver transplant recipients or in patients with chronic hepatitis B virus infection with decompensated liver disease.
2. Dosage and Administration
2.1 HIV Counseling and Testing
HIV counseling and testing should be offered to all patients before beginning treatment with EPIVIR-HBV and periodically during treatment because of the risk of emergence of resistant human immunodeficiency virus type 1 (HIV-1) and limitation of treatment options if EPIVIR-HBV is prescribed to treat chronic hepatitis B infection in a patient who has unrecognized HIV-1 infection or acquires HIV-1 infection during treatment [see Warnings and Precautions (5.2)].
2.2 Recommended Dosage for Adult Patients
The recommended oral dosage of EPIVIR‑HBV is 100 mg once daily.
2.3 Recommended Dosage for Pediatric Patients
The recommended oral dosage of EPIVIR‑HBV for pediatric patients aged 2 to 17 years is 3 mg per kg once daily up to a maximum daily dosage of 100 mg. The oral solution formulation should be prescribed for patients requiring a dosage less than 100 mg or if unable to swallow tablets.
2.4 Patients with Renal Impairment
Dosage recommendations for adult patients with reduced renal function are provided in Table 1 [see Clinical Pharmacology (12.3 )].
Creatinine Clearance (mL/min) | Recommended Dosage of EPIVIR-HBV |
≥50 | 100 mg once daily |
30-49 | 100 mg first dose, then 50 mg once daily |
15-29 | 100 mg first dose, then 25 mg once daily |
5-14 | 35 mg first dose, then 15 mg once daily |
<5 | 35 mg first dose, then 10 mg once daily |
Following correction of the dosage for renal impairment, no additional dosage modification of EPIVIR-HBV is required after routine (4-hour) hemodialysis or peritoneal dialysis [see Clinical Pharmacology (12.3 )].
There are insufficient data to recommend a specific dosage of EPIVIR-HBV in pediatric patients with renal impairment.
2.5 Important Administration Instructions
- EPIVIR-HBV tablets and oral solution may be administered with or without food.
- The tablets and oral solution may be used interchangeably [see Clinical Pharmacology (12.3)].
- The oral solution should be used for doses less than 100 mg.
- EPIVIR-HBV should not be used with other medications that contain lamivudine or medications that contain emtricitabine.
2.6 Assessing Patients during Treatment
Patients should be monitored regularly during treatment by a physician experienced in the management of chronic hepatitis B. During treatment, combinations of events such as return of persistently elevated alanine aminotransferase (ALT), increasing levels of HBV DNA over time after an initial decline below assay limit, progression of clinical signs or symptoms of hepatic disease, and/or worsening of hepatic necroinflammatory findings may be considered as potentially reflecting loss of therapeutic response. Such observations should be taken into consideration when determining the advisability of continuing therapy with EPIVIR-HBV.
The optimal duration of treatment, the durability of Hepatitis B e Antigen (HBeAg) seroconversions occurring during treatment, and the relationship between treatment response and long‑term outcomes such as hepatocellular carcinoma or decompensated cirrhosis are not known.
3. Dosage Forms and Strengths
4. Contraindications
5. Warnings and Precautions
5.1 Exacerbations of Hepatitis after Discontinuation of Treatment
Clinical and laboratory evidence of exacerbations of hepatitis have occurred after discontinuation of lamivudine. These exacerbations have been detected primarily by serum ALT elevations in addition to re-emergence of HBV DNA commonly observed after stopping treatment; see Table 4 for more information regarding frequency of posttreatment ALT elevations [see Adverse Reactions (6.1)]. Although most events appear to have been self-limited, fatalities have been reported in some cases. The causal relationship to discontinuation of lamivudine treatment is unknown. Patients should be closely monitored with both clinical and laboratory follow-up for at least several months after stopping treatment with EPIVIR-HBV. There is insufficient evidence to determine whether re-initiation of EPIVIR-HBV alters the course of posttreatment exacerbations of hepatitis.
5.2 Risk of HIV-1 Resistance if EPIVIR-HBV is Used in Patients with Unrecognized or Untreated HIV-1 Infection
EPIVIR-HBV tablets and oral solution contain a lower lamivudine dose than the lamivudine dose used to treat HIV-1 infection with EPIVIR tablets and oral solution or with lamivudine-containing antiretroviral fixed-dose combination products.
EPIVIR-HBV is not appropriate for patients co-infected with HBV and HIV-1. If a patient with unrecognized or untreated HIV-1 infection is prescribed EPIVIR-HBV for the treatment of HBV, rapid emergence of HIV-1 resistance is likely to result because of the subtherapeutic dose and the inappropriate use of monotherapy for HIV-1 treatment. HIV counseling and testing should be offered to all patients before beginning treatment with EPIVIR-HBV and periodically during treatment because of the risk of rapid emergence of resistant HIV-1 and limitation of treatment options if EPIVIR-HBV is prescribed to treat chronic hepatitis B in a patient who has unrecognized or untreated HIV-1 infection or who acquires HIV-1 infection during treatment.
5.3 Emergence of Resistance-Associated HBV Substitutions
In controlled clinical trials, YMDD‑mutant HBV was detected in subjects with on–EPIVIR-HBV re‑appearance of HBV DNA after an initial decline below the assay limit [see Microbiology (12.4)]. Subjects treated with EPIVIR-HBV (adults and children) with YMDD‑mutant HBV at 52 weeks showed diminished treatment responses in comparison with subjects treated with EPIVIR-HBV without evidence of YMDD substitutions, including the following: lower rates of HBeAg seroconversion and HBeAg loss (no greater than placebo recipients), more frequent return of positive HBV DNA, and more frequent ALT elevations. In the controlled trials, when subjects developed YMDD‑mutant HBV, they had a rise in HBV DNA and ALT from their previous on‑treatment levels. Progression of hepatitis B, including death, has been reported in some subjects with YMDD‑mutant HBV, including subjects from the liver transplant setting and from other clinical trials. In order to reduce the risk of resistance in patients receiving monotherapy with EPIVIR-HBV, a switch to an alternative regimen should be considered if serum HBV DNA remains detectable after 24 weeks of treatment. Optimal therapy should be guided by resistance testing.
5.4 Lactic Acidosis and Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues, including EPIVIR-HBV. A majority of these cases have been in women. Female sex and obesity may be risk factors for the development of lactic acidosis and severe hepatomegaly with steatosis in patients treated with antiretroviral nucleoside analogues. Most of these reports have described patients receiving nucleoside analogues for treatment of HIV infection, but there have been reports of lactic acidosis in patients receiving lamivudine for hepatitis B. Treatment with EPIVIR‑HBV should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations.
6. Adverse Reactions
The following adverse reactions are discussed in other sections of the labeling:
- Exacerbations of hepatitis B after discontinuation of treatment [see Warnings and Precautions (5.1)].
- Risk of emergence of resistant HIV-1 infection [see Warnings and Precautions (5.2)].
- Risk of emergence of resistant HBV infection [see Warnings and Precautions (5.3)].
- Lactic acidosis and severe hepatomegaly with steatosis [see Warnings and Precautions (5.4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Clinical Trials Experience in Adult Subjects with Chronic HBV Infection
Clinical adverse reactions (regardless of investigator’s causality assessment) reported in greater than or equal to 10% of subjects who received EPIVIR-HBV and reported at a rate greater than in subjects who received placebo are listed in Table 2.
| a Includes adverse events regardless of severity and causality assessment. | ||
Adverse Event | EPIVIR-HBV(n = 332) | Placebo(n = 200) |
Ear, Nose, and Throat | ||
Ear, nose, and throat infections | 25% | 21% |
Sore throat | 13% | 8% |
Gastrointestinal | ||
Diarrhea | 14% | 12% |
Specified laboratory abnormalities reported in subjects who received EPIVIR-HBV and reported at a rate greater than in subjects who received placebo are listed in Table 3.
| a Includes subjects treated for 52 to 68 weeks. b Includes observations during and after treatment in the 2 placebo-controlled trials that collected this information. ULN = Upper limit of normal. | |||||
Test(Abnormal Level) | Subjects with Abnormality/Subjects with Observations | ||||
EPIVIR-HBV | Placebo | ||||
Serum Lipase ≥2.5 x ULNb | 10% | 7% | |||
Creatine Phosphokinase (CPK) ≥7 x baseline | 9% | 5% | |||
Platelets <50,000/mm3 | 4% | 3% | |||
In subjects followed for up to 16 weeks after discontinuation of treatment, posttreatment ALT elevations were observed more frequently in subjects who had received EPIVIR-HBV than in subjects who had received placebo. A comparison of ALT elevations between Weeks 52 and 68 in subjects who discontinued EPIVIR-HBV at Week 52 and subjects in the same trials who received placebo throughout the treatment course is shown in Table 4.
| a Each subject may be represented in one or more category. b During treatment phase. c Comparable to a Grade 3 toxicity in accordance with modified WHO criteria. ULN = Upper limit of normal. | ||||||||
Abnormal Value | Subjects with ALT Elevation/Subjects with Observationsa | |||||||
EPIVIR-HBVb | Placebob | |||||||
ALT ≥2 x baseline value | 27% | 19% | ||||||
ALT ≥3 x baseline valuec | 21% | 8% | ||||||
ALT ≥2 x baseline value and absolute ALT >500 IU/L | 15% | 7% | ||||||
ALT ≥2 x baseline value; and bilirubin >2 x ULN and ≥2 x baseline value | 0.7% | 0.9% | ||||||
Clinical Trials Experience in Pediatric Subjects with Chronic HBV Infection
Most commonly observed adverse reactions in the pediatric trials were similar to those in adult trials. Posttreatment transaminase elevations were observed in some subjects followed after cessation of EPIVIR-HBV.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of EPIVIR-HBV. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to lamivudine.
Blood and Lymphatic
Anemia (including pure red cell aplasia and severe anemias progressing on therapy), lymphadenopathy, splenomegaly, thrombocytopenia.
Digestive
Stomatitis.
Endocrine and Metabolic
Hyperglycemia.
General
Weakness.
Hepatic and Pancreatic
Lactic acidosis and steatosis [see Warnings and Precautions (5.4)], posttreatment exacerbations of hepatitis [see Warnings and Precautions (5.1)], pancreatitis.
Hypersensitivity
Anaphylaxis, urticaria.
Musculoskeletal
Cramps, rhabdomyolysis.
Nervous
Paresthesia, peripheral neuropathy.
Respiratory
Abnormal breath sounds/wheezing.
Skin
Alopecia, pruritus, rash.
7. Drug Interactions
7.1 Drugs Inhibiting Organic Cation Transporters
Lamivudine is predominantly eliminated in the urine by active organic cationic secretion. The possibility of interactions with other drugs administered concurrently should be considered, particularly when their main route of elimination is active renal secretion via the organic cationic transport system (e.g., trimethoprim) [see Clinical Pharmacology (12.3)]. No data are available regarding interactions with other drugs that have renal clearance mechanisms similar to that of lamivudine.
7.2 Sorbitol
Coadministration of single doses of lamivudine and sorbitol resulted in a sorbitol dose-dependent reduction in lamivudine exposures. When possible, avoid use of sorbitol-containing medicines with lamivudine [see Clinical Pharmacology (12.3)]. Consider more frequent monitoring of HBV viral load when chronic coadministration cannot be avoided.
8. Use in Specific Populations
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to lamivudine during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Available data from the APR show no substantial difference in the risk of overall major birth defects for lamivudine compared with the background rate for major birth defects of 2.7% reported in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP). The APR uses the MACDP as a U.S. reference population for birth defects in the general population. The MACDP evaluates women and infants from a limited geographic area and does not include outcomes for births that occur at less than 20 weeks’ gestation. Of over 12,900 women exposed to lamivudine in the APR, less than 2% were HBV mono-infected. The majority of women exposed to lamivudine in the APR were HIV-1-infected and were treated with higher doses of lamivudine compared with HBV mono-infected women. In addition to lamivudine, HIV-1-infected women were also treated with other concomitant medications for HIV-1 infection (see Data). The estimated rate of miscarriage for women exposed to lamivudine in the indicated population is unknown. The estimated background rate of miscarriage in clinically recognized pregnancies in the U.S. general population is 15% to 20%.
Oral administration of lamivudine to pregnant rabbits during organogenesis resulted in embryolethality at systemic exposure (AUC) similar to the recommended clinical dose; however, no adverse developmental effects were observed with oral administration of lamivudine to pregnant rats during organogenesis at plasma concentrations (Cmax) 60 times the recommended clinical dose (see Data).
Data
Human Data: Based on prospective reports from the APR of over 12,900 exposures to lamivudine, during pregnancy resulting in live births (including over 5,400 exposed in the first trimester and over 7,500 exposed in the second/third trimester), there was no difference between the overall risk of birth defects with lamivudine compared with the background birth defect rate of 2.7% observed in the U.S. reference population of the MACDP. The prevalence of birth defects in live births was 3.1% (95% CI: 2.7% to 3.6%) following first trimester exposure to lamivudine-containing regimens and 2.9% (95% CI: 2.5% to 3.3%) following second/third trimester exposure to lamivudine-containing regimens.
The pharmacokinetics of lamivudine in patients with HBV or HIV-1 infection and in healthy volunteers are similar at similar doses. Lamivudine pharmacokinetics were studied in pregnant women with HIV-1 infection during 2 clinical trials conducted in South Africa. The trials assessed pharmacokinetics in 16 women at 36 weeks’ gestation using 150 mg lamivudine twice daily (3 times the recommended daily dosage for HBV) with zidovudine, 10 women at 38 weeks’ gestation using 150 mg lamivudine twice daily (3 times the recommended daily dosage for HBV) with zidovudine, and 10 women at 38 weeks’ gestation using lamivudine 300 mg twice daily (6 times the recommended daily dosage for HBV) without other antiretrovirals. Lamivudine concentrations were generally similar in maternal, neonatal, and umbilical cord serum samples. In a subset of subjects, amniotic fluid specimens were collected following natural rupture of membranes and confirmed that lamivudine crosses the placenta in humans. Based on limited data at delivery, median (range) amniotic fluid concentrations of lamivudine were 3.9- (1.2- to 12.8-) fold greater compared with paired maternal serum concentrations (n = 8).
Animal Data: Lamivudine was administered orally to pregnant rats (at 90, 600, and 4,000 mg per kg per day) and rabbits (at 90, 300, and 1,000 mg per kg per day and at 15, 40, and 90 mg per kg per day) during organogenesis (on Gestation Days 7 through 16 [rat] and 8 through 20 [rabbit]). No evidence of fetal malformations due to lamivudine was observed in rats and rabbits at doses producing plasma concentrations (Cmax) approximately 53 or more times higher than human exposure at the recommended daily dose. Evidence of early embryolethality in the absence of maternal toxicity was seen in the rabbit at systemic exposures (AUC) similar to those observed in humans, but there was no indication of this effect in the rat at plasma concentrations (Cmax) 60 times higher than human exposure at the recommended daily dose. Studies in pregnant rats showed that lamivudine is transferred to the fetus through the placenta. In the fertility/pre-and postnatal development study in rats, lamivudine was administered orally at doses of 180, 900, and 4,000 mg per kg per day (from prior to mating through postnatal Day 20). In the study, development of the offspring, including fertility and reproductive performance, was not affected by maternal administration of lamivudine at plasma concentrations (Cmax) 104 times higher than human exposure.
8.2 Lactation
Risk Summary
Lamivudine is present in human milk. There is no information available regarding lamivudine concentrations in milk from lactating women receiving lamivudine for treatment of HBV infection. However, in lactating women with HIV-1 infection being treated with lamivudine at 3 or 6 times the recommended daily dose for HBV, lamivudine concentrations in milk were similar to those observed in serum (see Data). The lamivudine dose received by a breastfed infant of a mother being treated for HIV-1 infection was estimated to be approximately 6% of the recommended daily lamivudine dose for HBV in children over 2 years of age.
There is no information available regarding the effects of the drug on the breastfed infant or on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for EPIVIR-HBV and any potential adverse effects on the breastfed infant from lamivudine or from the underlying maternal condition.
Data
In mothers with HIV receiving lamivudine monotherapy (300 mg twice daily [6 times the recommended daily dosage for HBV]) or combination therapy (150 mg lamivudine twice daily [3 times the recommended daily dosage for HBV] with 300 mg zidovudine twice daily), the median breast milk to plasma lamivudine concentration ratio was 0.6 to 3.3, and the estimated infant daily dose was approximately 6% of the recommended 3-mg-per-kg daily lamivudine dose for treatment of HBV in children over 2 years of age. In breastfed infants of mothers with HIV-1 infection receiving lamivudine therapy, the blood concentrations of lamivudine decreased after delivery and were undetectable at 6 months despite constant milk concentrations. This is consistent with increased lamivudine renal clearance in the first 6 months of life.
8.4 Pediatric Use
EPIVIR-HBV is indicated for the treatment of chronic hepatitis B virus infection in pediatric patients aged 2 to 17 years [see Indications and Usage (1), Clinical Pharmacology (12.3), Clinical Studies (14.2)]. The safety and efficacy of EPIVIR-HBV in pediatric patients younger than 2 years have not been established.
8.5 Geriatric Use
Clinical trials of EPIVIR-HBV did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, caution should be exercised in the administration of EPIVIR-HBV in elderly patients reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)].
10. Overdosage
There is no known specific treatment for overdose with EPIVIR-HBV. If overdose occurs, the patient should be monitored and standard supportive treatment applied, as required. Because a negligible amount of lamivudine was removed via (4-hour) hemodialysis, continuous ambulatory peritoneal dialysis, and automated peritoneal dialysis, it is not known if continuous hemodialysis would provide clinical benefit in a lamivudine overdose event.
11. Description
EPIVIR-HBV is a synthetic nucleoside analogue with activity against HBV. The chemical name of lamivudine is (2R,cis)-4-amino-1-(2-hydroxymethyl-1,3-oxathiolan-5-yl)-(1H)-pyrimidin-2-one. Lamivudine is the (-)enantiomer of a dideoxy analogue of cytidine. Lamivudine has also been referred to as (-)2′,3′-dideoxy, 3′-thiacytidine. It has a molecular formula of C8H11N3O3S and a molecular weight of 229.3 g per mol. It has the following structural formula:
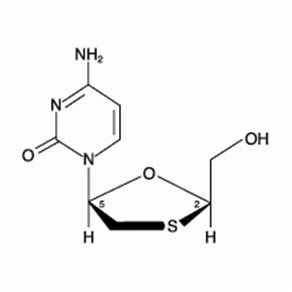
Lamivudine is a white to off-white crystalline solid with a solubility of approximately 70 mg per mL in water at 20°C.
EPIVIR-HBV tablets are for oral administration. Each tablet contains 100 mg of lamivudine and the inactive ingredients hypromellose, macrogol 400, magnesium stearate, microcrystalline cellulose, polysorbate 80, red iron oxide, sodium starch glycolate, titanium dioxide, and yellow iron oxide.
EPIVIR-HBV oral solution is for oral administration. One milliliter (1 mL) of EPIVIR-HBV oral solution contains 5 mg of lamivudine (5 mg per mL) in an aqueous solution and the inactive ingredients artificial strawberry and banana flavors, citric acid (anhydrous), methylparaben, propylene glycol, propylparaben, sodium citrate (dihydrate), and sucrose (200 mg).
12. Clinical Pharmacology
12.1 Mechanism of Action
Lamivudine is an antiviral agent with activity against HBV [see Microbiology (12.4)].
12.3 Pharmacokinetics
Pharmacokinetics in Adults
The pharmacokinetic properties of lamivudine have been studied as single and multiple oral doses ranging from 5 mg to 600 mg per day administered to HBV-infected subjects.
Absorption and Bioavailability: Following single oral doses of 100 mg, the peak serum lamivudine concentration (Cmax) in HBV-infected patients (steady state) and healthy subjects (single dose) was 1.28 ± 0.56 mcg per mL and 1.05 ± 0.32 mcg per mL (mean ± SD), respectively, which occurred between 0.5 and 2 hours after administration. The area under the plasma concentration versus time curve (AUC[0-24 h]) following 100-mg lamivudine oral single and repeated daily doses to steady state was 4.3 ± 1.4 (mean ± SD) and 4.7 ± 1.7 mcg•hour per mL, respectively. The relative bioavailability of the tablet and oral solution were demonstrated in healthy subjects. Although the solution demonstrated a slightly higher peak serum concentration (Cmax), there was no significant difference in systemic exposure (AUC) between the oral solution and the tablet. Therefore, the oral solution and the tablet may be used interchangeably.
After oral administration of lamivudine once daily to HBV-infected adults, the AUC and Cmax increased in proportion to dose over the range from 5 mg to 600 mg once daily.
Absolute bioavailability in 12 adult subjects was 86% ± 16% (mean ± SD) for the 150-mg tablet and 87% ± 13% for the 10-mg-per mL oral solution.
Effects of Food on Oral Absorption: EPIVIR-HBV tablets and oral solution may be administered with or without food. The 100-mg tablet was administered orally to 24 healthy subjects on 2 occasions, once in the fasted state and once with food (standard meal: 967 kcal; 67 grams fat, 33 grams protein, 58 grams carbohydrate). There was no significant difference in systemic exposure (AUC) in the fed and fasted states.
Distribution: The apparent volume of distribution after IV administration of lamivudine to 20 HIV-1-infected subjects was 1.3 ± 0.4 L per kg, suggesting that lamivudine distributes into extravascular spaces. Volume of distribution was independent of dose and did not correlate with body weight.
Binding of lamivudine to human plasma proteins is less than 36%. In vitro studies showed that over the concentration range of 0.1 to 100 mcg per mL, the amount of lamivudine associated with erythrocytes ranged from 53% to 57% and was independent of concentration.
Metabolism: Metabolism of lamivudine is a minor route of elimination. In humans, the only known metabolite of lamivudine is the trans-sulfoxide metabolite (approximately 5% of an oral dose after 12 hours). Serum concentrations of this metabolite have not been determined. Lamivudine is not significantly metabolized by cytochrome P450 enzymes.
Elimination: The majority of lamivudine is eliminated unchanged in urine by active organic cationic secretion. In 9 healthy subjects given a single 300-mg oral dose of lamivudine, renal clearance was 199.7 ± 56.9 mL per min (mean ± SD). In 20 HIV-1-infected subjects given a single IV dose, renal clearance was 280.4 ± 75.2 mL per min (mean ± SD), representing 71% ± 16% (mean ± SD) of total clearance of lamivudine.
In most single-dose trials with plasma sampling for up to 48 or 72 hours after dosing, the observed mean elimination half-life (t½) ranged from 13 to 19 hours. In HIV-1-infected subjects, total clearance was 398.5 ± 69.1 mL per min (mean ± SD). Oral clearance and elimination half-life were independent of dose and body weight over an oral dosing range of 0.25 to 10 mg per kg.
Specific Populations
Patients with Renal Impairment: The pharmacokinetic properties of lamivudine have been determined in healthy adults and in adults with impaired renal function, with and without hemodialysis (Table 5).
Parameter | Creatinine Clearance Criterion (Number of Subjects) | ||
≥80 mL/min (n = 9) | 20-59 mL/min (n = 8) | <20 mL/min (n = 6) | |
Creatinine clearance (mL/min) | 97 (range 82-117) | 39 (range 25-49) | 15 (range 13-19) |
Cmax (mcg/mL) | 1.31 ± 0.35 | 1.85 ± 0.40 | 1.55 ± 0.31 |
AUC (mcg•h/mL) | 5.28 ± 1.01 | 14.67 ± 3.74 | 27.33 ± 6.56 |
Cl/F (mL/min) | 326.4 ± 63.8 | 120.1 ± 29.5 | 64.5 ± 18.3 |
Tmax was not significantly affected by renal function. Based on these observations, it is recommended that the dosage of lamivudine be modified in patients with renal impairment [see Dosage and Administration (2.4)].
Hemodialysis increases lamivudine clearance from a mean of 64 to 88 mL per min; however, the length of time of hemodialysis (4 hours) was insufficient to significantly alter mean lamivudine exposure after a single-dose administration. Continuous ambulatory peritoneal dialysis and automated peritoneal dialysis have negligible effects on lamivudine clearance. Therefore, it is recommended, following correction of dose for creatinine clearance, that no additional dose modification be made after routine hemodialysis or peritoneal dialysis.
The effects of renal impairment on lamivudine pharmacokinetics in pediatric patients with chronic hepatitis B is not known.
Patients with Hepatic Impairment: The pharmacokinetic properties of lamivudine in adults with hepatic impairment are shown in Table 6. Subjects were stratified by severity of hepatic impairment.
| a Hepatic impairment assessed by aminopyrine breath test. | |||||||
Parameter | Normal (n = 8) | Impairmenta | |||||
Moderate (n = 8) | Severe (n = 8) | ||||||
Cmax (mcg/mL) | 0.92 ± 0.31 | 1.06 ± 0.58 | 1.08 ± 0.27 | ||||
AUC (mcg•h/mL) | 3.96 ± 0.58 | 3.97 ± 1.36 | 4.30 ± 0.63 | ||||
Tmax (h) | 1.3 ± 0.8 | 1.4 ± 0.8 | 1.4 ± 1.2 | ||||
Cl/F (mL/min) | 424.7 ± 61.9 | 456.9 ± 129.8 | 395.2 ± 51.8 | ||||
Clr (mL/min) | 279.2 ± 79.2 | 323.5 ± 100.9 | 216.1 ± 58.0 | ||||
Pharmacokinetic parameters were not altered by diminishing hepatic impairment. Safety and efficacy of EPIVIR-HBV have not been established in the presence of decompensated liver disease [see Indications and Usage (1)].
Patients Post-Hepatic Transplant: Fourteen HBV-infected adult subjects received liver transplant following lamivudine therapy and completed pharmacokinetic assessments at enrollment, 2 weeks after 100-mg once-daily dosing (pre-transplant), and 3 months following transplant; there were no significant differences in pharmacokinetic parameters. The overall exposure of lamivudine is primarily affected by renal impairment; consequently, transplant patients with renal impairment had generally higher exposure than patients with normal renal function. Safety and efficacy of EPIVIR-HBV have not been established in this population [see Indications and Usage (1)].
Pregnant Women: The pharmacokinetics of lamivudine in patients with HBV or HIV-1 infection and in healthy volunteers were similar at similar doses. Lamivudine pharmacokinetics were studied in 36 pregnant women with HIV during 2 clinical trials conducted in South Africa (3 to 6 times the recommended daily dosage for HBV). Lamivudine pharmacokinetics in pregnant women were similar to those seen in non-pregnant adults and in postpartum women. Lamivudine concentrations were generally similar in maternal, neonatal, and umbilical cord serum samples.
Pediatric Patients: Lamivudine pharmacokinetics were evaluated in a 28-day dose-ranging trial in 53 pediatric subjects with chronic hepatitis B. Subjects aged 2 to 12 years were randomized to receive lamivudine 0.35 mg per kg twice daily, 3 mg per kg once daily, 1.5 mg per kg twice daily, or 4 mg per kg twice daily. Subjects aged 13 to 17 years received lamivudine 100 mg once daily. Lamivudine Tmax was 0.5 to 1 hour. In general, both Cmax and exposure (AUC) showed dose proportionality in the dosing range studied. Weight-corrected oral clearance was highest at age 2 and declined from 2 to 12 years, where values were then similar to those seen in adults. A dose of 3 mg per kg given once daily produced a steady-state lamivudine AUC (mean 5,953 ng•hour per mL ± 1,562 SD) similar to that associated with a dose of 100 mg per day in adults.
Geriatric Patients: The pharmacokinetics of lamivudine after administration of EPIVIR-HBV to subjects over 65 years have not been studied [see Use in Specific Populations (8.5)].
Male and Female Patients: There are no significant or clinically relevant gender differences in lamivudine pharmacokinetics.
Racial Groups: There are no significant or clinically relevant racial differences in lamivudine pharmacokinetics.
Drug Interaction Studies
Effect of Lamivudine on the Pharmacokinetics of Other Agents: Based on in vitro study results, lamivudine at therapeutic drug exposures is not expected to affect the pharmacokinetics of drugs that are substrates of the following transporters: organic anion transporter polypeptide 1B1/3 (OATP1B1/3), breast cancer resistance protein (BCRP), P-glycoprotein (P-gp), multidrug and toxin extrusion protein 1 (MATE1), MATE2-K, organic cation transporter 1 (OCT1), OCT2, or OCT3.
Effect of Other Agents on the Pharmacokinetics of Lamivudine: Lamivudine is a substrate of MATE1, MATE2-K, and OCT2 in vitro. Trimethoprim (an inhibitor of these drug transporters) has been shown to increase lamivudine plasma concentrations. This interaction is not considered clinically significant, and no dose adjustment of lamivudine is needed.
Lamivudine is a substrate of P-gp and BCRP; however, considering its absolute bioavailability (87%), it is unlikely that these transporters play a significant role in the absorption of lamivudine. Therefore, coadministration of drugs that are inhibitors of these efflux transporters is unlikely to affect the disposition and elimination of lamivudine.
Interferon Alfa: There was no significant pharmacokinetic interaction between lamivudine and interferon alfa in a trial of 19 healthy male subjects.
Ribavirin: In vitro data indicate ribavirin reduces phosphorylation of lamivudine, stavudine, and zidovudine. However, no pharmacokinetic (e.g., plasma concentrations or intracellular triphosphorylated active metabolite concentrations) or pharmacodynamic (e.g., loss of HIV-1/HCV virologic suppression) interaction was observed when ribavirin and lamivudine (n = 18), stavudine (n = 10), or zidovudine (n = 6) were coadministered as part of a multi-drug regimen to HIV‑1/HCV co-infected subjects.
Sorbitol (Excipient): Lamivudine and sorbitol solutions were coadministered to 16 healthy adult subjects in an open-label, randomized sequence, 4-period, crossover trial. Each subject received a single 300-mg dose of lamivudine oral solution alone or coadministered with a single dose of 3.2 grams, 10.2 grams, or 13.4 grams of sorbitol in solution. Coadministration of lamivudine with sorbitol resulted in dose-dependent decreases of 20%, 39%, and 44% in the AUC(0-24), 14%, 32%, and 36% in the AUC(∞), and 28%, 52%, and 55% in the Cmax of lamivudine.
Trimethoprim/Sulfamethoxazole: Lamivudine and trimethoprim/sulfamethoxazole (TMP/SMX) were coadministered to 14 HIV-1-positive subjects in a single-center, open-label, randomized, crossover trial. Each subject received treatment with a single 300-mg dose of lamivudine and TMP 160 mg/SMX 800 mg once a day for 5 days with concomitant administration of lamivudine 300 mg with the fifth dose in a crossover design. Coadministration of TMP/SMX with lamivudine resulted in an increase of 43% ± 23% (mean ± SD) in lamivudine AUC(∞), a decrease of 29% ± 13% in lamivudine oral clearance, and a decrease of 30% ± 36% in lamivudine renal clearance. The pharmacokinetic properties of TMP and SMX were not altered by coadministration with lamivudine.
Zidovudine: No clinically significant alterations in lamivudine or zidovudine pharmacokinetics were observed in 12 asymptomatic HIV-1‑infected adult subjects given a single dose of zidovudine (200 mg) in combination with multiple doses of lamivudine (300 mg every 12 hours).
12.4 Microbiology
Mechanism of Action
Lamivudine is a synthetic nucleoside analogue. Intracellularly, lamivudine is phosphorylated to its active 5′-triphosphate metabolite, lamivudine triphosphate (3TC-TP). The principal mode of action of 3TC-TP is inhibition of the RNA- and DNA-dependent polymerase activities of HBV reverse transcriptase (rt) via DNA chain termination after incorporation of the nucleotide analogue.
Antiviral Activity
Activity of lamivudine against HBV in cell culture was assessed in HBV DNA‑transfected 2.2.15 cells, HB611 cells, and infected human primary hepatocytes. EC50 values (the concentration of drug needed to reduce the level of extracellular HBV DNA by 50%) varied from 0.01 microM (2.3 ng per mL) to 5.6 microM (1,288 ng per mL) depending upon the duration of exposure of cells to lamivudine, the cell model system, and the protocol used. See the prescribing information for EPIVIR regarding activity of lamivudine against HIV. The anti-HBV activity of lamivudine in combination with adefovir or tenofovir in cell culture was not antagonistic.
Resistance
Lamivudine‑resistant isolates have been identified in subjects with virologic breakthrough.
Lamivudine‑resistant HBV isolates develop rtM204V/I substitutions in the YMDD motif of the catalytic domain of the viral reverse transcriptase. rtM204V/I substitutions are frequently accompanied by other substitutions (rtV173L, rtL180M) which enhance the level of lamivudine resistance or act as compensatory substitutions improving replication efficiency. Other substitutions reported in lamivudine‑resistant HBV isolates include rtH55R, rtL80I/V, rtV173M, rtA181T/V, rtT184S, rtF219Y, rtL229F/M/V/W, and rtQ267H.
In 4 controlled clinical trials evaluating EPIVIR-HBV in adults with HBeAg‑positive chronic hepatitis B virus infection (CHB), YMDD‑mutant HBV was detected in 81 of 335 subjects receiving EPIVIR-HBV 100 mg once daily for 52 weeks. The prevalence of YMDD substitutions was less than 10% in each of these trials for subjects studied at 24 weeks and increased to an average of 24% (range in 4 trials: 16% to 32%) at 52 weeks. A similar prevalence of YMDD substitutions has been reported in large controlled Phase 3 clinical trials utilizing EPIVIR-HBV as a comparator arm in adults with HBeAg-positive CHB for 48 weeks (range in 4 trials: 11% to 27%) and in adults with HBeAg-negative CHB for 48 weeks (range in 3 clinical trials: 6% to 18%).
Long-term follow up in subjects who continued 100 mg per day of EPIVIR-HBV demonstrated that the prevalence of YMDD substitutions further increased from 23% (211 of 998) in Year 1, to 46% (368 of 796), 55% (378 of 688), 71% (421 of 592), and 65% (103 of 159) in Years 2, 3, 4, and 5, respectively.
In a controlled trial, treatment‑naive subjects with HBeAg‑positive CHB were treated with EPIVIR-HBV or EPIVIR-HBV plus adefovir dipivoxil combination therapy. Following 104 weeks of therapy, YMDD‑mutant HBV was detected in 7 of 40 (18%) subjects receiving combination therapy compared with 15 of 35 (43%) subjects receiving therapy with only EPIVIR-HBV. In 2 controlled clinical trials, treatment-naive subjects who received 48 weeks of therapy with EPIVIR-HBV in combination with pegylated interferon developed YMDD substitutions less frequently than subjects treated with EPIVIR-HBV alone (1 of 173 [1%] versus 32 of 179 [18%] in HBeAg-negative subjects; 9 of 256 [4%] versus 69 of 254 [27%] in HBeAg-positive subjects).
Several clinical studies have evaluated alternative regimens in subjects who failed EPIVIR-HBV due to development of lamivudine resistance. These studies demonstrated a higher rate of viral suppression and decreased development of viral resistance compared with continuation of monotherapy with EPIVIR-HBV.
Pediatric Subjects: In a controlled trial in pediatric subjects, YMDD-mutant HBV was detected in 31 of 166 (19%) subjects receiving EPIVIR-HBV for 52 weeks. For a subgroup that remained on therapy with EPIVIR-HBV in a follow-up trial, YMDD substitutions increased from 24% (29 of 121) at 12 months to 59% (68 of 115) at 24 months and 64% (66 of 103) at 36 months of treatment with EPIVIR-HBV.
Cross-Resistance
HBV containing lamivudine resistance-associated substitutions (rtL180M, rtM204I, rtM204V, rtL180M and rtM204V, rtV173L and rtL180M and rtM204V) retain susceptibility to adefovir dipivoxil but have reduced susceptibility to entecavir (greater than 30-fold) and telbivudine (greater than 100-fold). The lamivudine resistance-associated substitution rtA181T results in diminished response to adefovir and telbivudine. Similarly, HBV with entecavir resistance-associated substitutions (rtI169T and rtM250V, rtT184G and rtS202I) have greater than 1,000-fold reductions in susceptibility to lamivudine.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term carcinogenicity studies with lamivudine in mice and rats showed no evidence of carcinogenic potential at exposures up to 34 times (mice), and 113 and 187 times (male and female rats, respectively) those observed in humans at the recommended therapeutic dose for chronic hepatitis B.
Mutagenesis
Lamivudine was mutagenic in an L5178Y mouse lymphoma assay and clastogenic in a cytogenetic assay using cultured human lymphocytes. Lamivudine was not mutagenic in a microbial mutagenicity assay, in an in vitro cell transformation assay, in a rat micronucleus test, in a rat bone marrow cytogenetic assay, and in an assay for unscheduled DNA synthesis in rat liver.
Impairment of Fertility
Lamivudine did not affect male or female fertility in rats at oral doses up to 4,000 mg per kg per day, associated with concentrations approximately 70 times (male) or 104 times (females) higher than the concentrations (Cmax) in humans at the dose of 100 mg [see Use in Specific Populations (8.1)].
14. Clinical Studies
14.1 Adult Subjects
The safety and efficacy of EPIVIR-HBV 100 mg once daily versus placebo were evaluated in 3 controlled trials in subjects with compensated chronic hepatitis B virus infection. All subjects were aged 16 years or older and had chronic hepatitis B virus infection (serum HBsAg-positive for at least 6 months) accompanied by evidence of HBV replication (serum HBeAg-positive and positive for serum HBV DNA) and persistently elevated ALT levels and/or chronic inflammation on liver biopsy compatible with a diagnosis of chronic viral hepatitis. The results of these trials are summarized below.
- Trial 1 was a randomized, double-blind trial of EPIVIR-HBV 100 mg once daily versus placebo for 52 weeks followed by a 16-week no-treatment period in 141 treatment-naive U.S. subjects.
- Trial 2 was a randomized, double-blind, 3-arm trial that compared EPIVIR-HBV 25 mg once daily versus EPIVIR-HBV 100 mg once daily versus placebo for 52 weeks in 358 Asian subjects.
- Trial 3 was a randomized, partially-blind trial conducted primarily in North America and Europe in 238 subjects who had ongoing evidence of active chronic hepatitis B despite previous treatment with interferon alfa. The trial compared EPIVIR-HBV 100 mg once daily for 52 weeks, followed by either EPIVIR-HBV 100 mg or matching placebo once daily for 16 weeks (Arm 1), versus placebo once daily for 68 weeks (Arm 2).
Principal endpoint comparisons for the histologic and serologic outcomes in subjects receiving EPIVIR-HBV (100 mg daily) or placebo in these trials are shown in the following tables.
| a Improvement was defined as a greater than or equal to 2-point decrease in the Knodell Histologic Activity Index (HAI) at Week 52 compared with pretreatment HAI. Subjects with missing data at baseline were excluded. | ||||||
Assessment | Trial 1 | Trial 2 | Trial 3 | |||
EPIVIR- HBV (n = 62) | Placebo (n = 63) | EPIVIR-HBV (n = 131) | Placebo (n = 68) | EPIVIR-HBV (n = 110) | Placebo (n = 54) | |
Improvementa | 55% | 25% | 56% | 26% | 56% | 26% |
No Improvement | 27% | 59% | 36% | 62% | 25% | 54% |
Missing Data | 18% | 16% | 8% | 12% | 19% | 20% |
| a Three-component seroconversion was defined as Week 52 values showing loss of HBeAg, gain of HBeAb, and reduction of HBV DNA to below the solution-hybridization assay limit. Subjects with negative baseline HBeAg or HBV DNA assay were excluded from the analysis. | |||||||||||||
Seroconversion | Trial 1 | Trial 2 | Trial 3 | ||||||||||
EPIVIR- HBV (n = 63) | Placebo (n = 69) | EPIVIR- HBV (n = 140) | Placebo (n = 70) | EPIVIR- HBV (n = 108) | Placebo (n = 53) | ||||||||
Seroconverters | 17% | 6% | 16% | 4% | 15% | 13% | |||||||
Normalization of serum ALT levels was more frequent with treatment of EPIVIR-HBV compared with placebo in Trials 1, 2, and 3.
The majority of subjects treated with EPIVIR-HBV showed a decrease of HBV DNA to below the assay limit early in the course of therapy. However, reappearance of assay-detectable HBV DNA during treatment with EPIVIR-HBV was observed in approximately one-third of subjects after this initial response.
14.2 Pediatric Subjects
The safety and efficacy of EPIVIR-HBV were evaluated in a double-blind clinical trial in 286 subjects aged 2 to 17 years, who were randomized (2:1) to receive 52 weeks of EPIVIR-HBV (3 mg per kg once daily to a maximum of 100 mg once daily) or placebo. All subjects had compensated chronic hepatitis B accompanied by evidence of hepatitis B virus replication (positive serum HBeAg and positive for serum HBV DNA by a research branched-chain DNA assay) and persistently elevated serum ALT levels. The combination of loss of HBeAg and reduction of HBV DNA to below the assay limit of the research assay, evaluated at Week 52, was observed in 23% of subjects treated with EPIVIR-HBV and 13% of placebo-treated subjects. Normalization of serum ALT was achieved and maintained to Week 52 more frequently in subjects treated with EPIVIR-HBV compared with placebo (55% versus 13%). As in the adult controlled trials, most subjects treated with EPIVIR-HBV had decreases in HBV DNA below the assay limit early in treatment, but about one-third of subjects with this initial response had reappearance of assay-detectable HBV DNA during treatment. Adolescents (aged 13 to 17 years) showed less evidence of treatment effect than younger pediatric subjects.
16. How Supplied/Storage and Handling
EPIVIR-HBV tablets contain 100 mg of lamivudine, are butterscotch-colored, film-coated, biconvex, capsule-shaped tablets imprinted with “GX CG5” on one side. Packaged as follows:
Bottles of 60 tablets (NDC 0173-0662-00) with child-resistant closure.
Store EPIVIR-HBV tablets at 25°C (77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature].
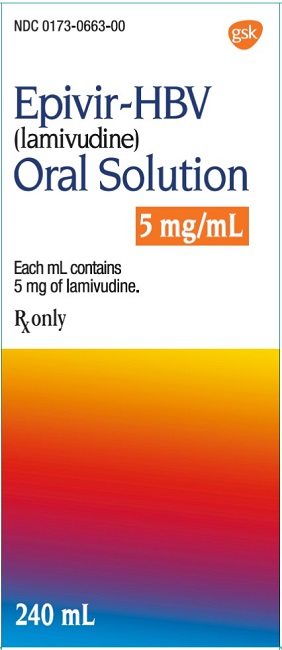
EPIVIR‑HBV oral solution is a clear, colorless to pale yellow, strawberry‑banana-flavored liquid. Each mL of the solution contains 5 mg of lamivudine. Packaged as follows:
Plastic bottles of 240 mL (NDC 0173-0663-00) with child-resistant closure. This product does not require reconstitution.
Store EPIVIR-HBV oral solution at controlled room temperature of 20°C to 25°C (68°F to 77°F) (see USP) in tightly closed bottles.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Severe Acute Exacerbation of Hepatitis after Discontinuation of Treatment
Inform patients that discontinuation of anti-hepatitis B therapy, including EPIVIR-HBV, may result in severe acute exacerbations of hepatitis B including decompensation of liver disease. Advise patients not to discontinue EPIVIR-HBV without first informing their healthcare provider [see Warnings and Precautions (5.1)].
Risk of Development of HIV-1 Resistance in Patients with HIV-1 Co-infection
Counsel patients on the importance of testing for HIV to avoid inappropriate therapy and development of resistance to HIV. HIV counseling and testing should be offered before starting EPIVIR-HBV and periodically during therapy. Inform patients that if they have or develop HIV infection and are not receiving effective HIV treatment, EPIVIR-HBV may increase the risk of development of resistance to HIV medications. Advise patients that EPIVIR-HBV contains a lower dose of the same active ingredient (lamivudine) as HIV drugs containing lamivudine [see Dosage and Administration (2.1), Warnings and Precautions (5.2)].
Emergence of HBV Resistance
Inform patients that emergence of resistant hepatitis B virus and worsening of disease can occur during treatment. Patients should promptly report any new or worsening symptoms to their physician [see Warnings and Precautions (5.3)].
Lactic Acidosis/Severe Hepatomegaly with Steatosis
Advise patients that lactic acidosis and severe hepatomegaly with steatosis have been reported with use of nucleoside analogues and other antiretrovirals. Advise patients to stop taking EPIVIR-HBV if they develop clinical symptoms suggestive of lactic acidosis or pronounced hepatotoxicity [see Warnings and Precautions (5.4)].
Hepatitis B Transmission
Advise patients that treatment with EPIVIR‑HBV has not been shown to reduce the risk of transmission of HBV to others through sexual contact or blood contamination.
Drug Interactions
Inform patients that EPIVIR-HBV may interact with some drugs; therefore, patients should be advised to report to their healthcare provider the use of any prescription or non-prescription medication or herbal products. Advise patients to avoid chronic use of sorbitol-containing prescription and over-the-counter medicines when possible. Taking EPIVIR-HBV with chronically administered sorbitol-containing medicines may decrease the concentrations of lamivudine [see Drug Interactions (7.2)].
Sucrose Content of EPIVIR-HBV Oral Solution
Advise diabetic patients that each 20‑mL dose of EPIVIR‑HBV oral solution contains 4 grams of sucrose (1 mL = 200 mg of sucrose) [see Description (11)].
Pregnancy Registry
Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to EPIVIR-HBV during pregnancy [see Use in Specific Populations (8.1)].
Missed Dosage
Instruct patients that if they miss a dose of EPIVIR-HBV, to take it as soon as they remember. Advise patients not to double their next dose or take more than the prescribed dose [see Dosage and Administration (2)].
EPIVIR‑HBV is a trademark owned by or licensed to the GSK group of companies.
EPIVIR is a trademark owned by or licensed to the ViiV Healthcare group of companies.
Distributed by:
GlaxoSmithKlineResearch Triangle Park, NC 27709
©2021 GSK group of companies or its licensor.
EPH:9PI
Patient Package Insert
PHARMACIST‑DETACH HERE AND GIVE INSTRUCTIONS TO PATIENT
PATIENT INFORMATION | ||
EPIVIR-HBV (EP-i-veer h-b-v) (lamivudine) tablets | EPIVIR-HBV (EP-i-veer h-b-v) (lamivudine) oral solution | |
What is the most important information I should know about EPIVIR‑HBV? EPIVIR-HBV can cause serious side effects, including: | ||
| ||
What is EPIVIR-HBV? EPIVIR‑HBV is a prescription medicine used to treat long-term (chronic) hepatitis B virus (HBV) when the disease is progressing and there is liver swelling (inflammation). It is not known if EPIVIR-HBV is safe and effective in:
EPIVIR-HBV does not stop you from spreading HBV to others by sex, sharing needles, or being exposed to your blood. Avoid doing things that can spread HBV infection to others. | ||
Do not take EPIVIR-HBV:
| ||
Before taking EPIVIR-HBV, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some medicines interact with EPIVIR-HBV. Keep a list of your medicines to show your healthcare provider and pharmacist.
EPIVIR-HBV should not be taken if you also take other medicines that contain lamivudine or emtricitabine. | ||
How should I take EPIVIR-HBV?
| ||
What are the possible side effects of EPIVIR-HBV? EPIVIR-HBV may cause serious side effects, including:
| ||
|
| |
| ||
|
| |
You may be more likely to get lactic acidosis or severe liver problems if you are female or very overweight (obese). The most common side effects of EPIVIR-HBV include ear, nose, and throat infections; sore throat; and diarrhea. Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of EPIVIR-HBV. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | ||
How should I store EPIVIR-HBV?
Keep EPIVIR-HBV and all medicines out of the reach of children. | ||
General information about the safe and effective use of EPIVIR-HBV Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use EPIVIR-HBV for a condition for which it was not prescribed. Do not give EPIVIR-HBV to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about EPIVIR-HBV that is written for health professionals. For more information call 1-888-825-5249. | ||
What are the ingredients in EPIVIR‑HBV? Active ingredient: lamivudine Inactive ingredients: EPIVIR-HBV tablets: hypromellose, macrogol 400, magnesium stearate, microcrystalline cellulose, polysorbate 80, red iron oxide, sodium starch glycolate, titanium dioxide, and yellow iron oxide. EPIVIR-HBV oral solution: artificial strawberry and banana flavors, citric acid (anhydrous), methylparaben, propylene glycol, propylparaben, sodium citrate (dihydrate), and sucrose (200 mg per mL). Trademarks are owned by or licensed to the GSK group of companies. Distributed by: GlaxoSmithKline, Research Triangle Park, NC 27709 ©2021 GSK group of companies or its licensor. EPH:9PIL | ||
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 12/2021
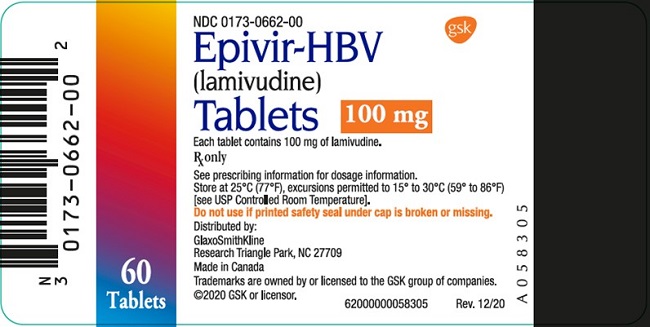
Package Label. Principal Display Panel
PRINCIPAL DISPLAY PANEL
NDC 0173-0662-00
Epivir-HBV
(lamivudine)
Tablets
100 mg
60 Tablets
Each tablet contains 100 mg of lamivudine.
Rx only
See prescribing information for dosage information.
Store at 25oC (77oF); excursions permitted to 15o to 30oC (59o to 86oF) [see USP Controlled Room Temperature].
Do not use if printed safety seal under cap is broken or missing.
Distributed by:
GlaxoSmithKline
Research Triangle Park, NC 27709\
Made in Canada
Trademarks are owned by or licensed to the GSK group of companies.
©2020 GSK or licensor.
- 62000000058305 Rev. 12/20