recommendations for Hepatitis B Screening and Testing in the United States
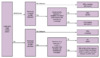
Multiple organizations in the United States have recommended performing routine screening for hepatitis B virus (HBV) infection for persons who are at increased risk of acquiring HBV, including the Centers for Disease Control and Prevention (CDC), the U.S. Preventive Services Task Force (USPSTF), the American Association for the Study of Liver Diseases (AASLD), and the American College of Physicians (ACP) [1,2,3,4] In March 2023, the CDC issued hepatitis B screening and testing guidance that recommends universal hepatitis B virus (HBV) screening for all adults, as well as risk-based and repeat testing for selected groups, utilizing a 3-test panel, which includes hepatitis B surface antigen (HBsAg), antibody to hepatitis B surface antigen (anti-HBs), and total antibody to hepatitis B core antigen (anti-HBc).[5] In these recommendations, the term “screening” refers to conducting serologic testing of asymptomatic persons not known to be at increased risk for exposure to HBV; the term “testing” refers to conducting serologic testing of persons with HBV-related symptoms or who have increased risk for HBV.[5] The following list summarizes the new CDC draft recommendations.[5] Note that certain indications for screening depend on country-level HBV prevalence (Table 1).[3]
Universal Hepatitis B Screening
- Universal HBV screening in all adults 18 years of age or older at least once in a lifetime.
- The HBV testing should consist of HBsAg, anti-HBs, and anti-HBc.
- For persons undergoing universal hepatitis B screening, repeat testing does not need to occur if no subsequent risk for HBV acquisition occurs following screening with the 3-test panel.
Screening Pregnant Women
- HBV screening for all pregnant women during each pregnancy, preferably in the first trimester, regardless of vaccination status or prior screening history.
- The HBV testing should consist of HBsAg, anti-HBs, and anti-HBc.
Risk-based Testing
- HBV testing should be performed for all individuals at increased risk for HBV, regardless of age, provided they were susceptible to HBV at the time of increased risk.
- Periodic, repeat testing should be performed for susceptible persons with ongoing risk factors, regardless of age.
Definition for HBV Susceptible
- The CDC defines susceptible persons to be those who
- Have never been infected with HBV (e.g., HBsAg negative and anti-HBc negative),
AND - Have not received a hepatitis B vaccine that is licensed in the United States or are known to be vaccine nonresponders.
- Have never been infected with HBV (e.g., HBsAg negative and anti-HBc negative),
Definition of Increased Risk for HBV Infection
- The CDC identifies the following groups of people to be at increased risk for HBV:
-
Persons currently or formerly incarcerated in jail, prison, or another detention setting
-
Persons with current or past sexually transmitted infections (STIs) or multiple sex partners
-
Persons with current or past hepatitis C virus (HCV) infection
-
Persons born in regions with an HBV prevalence equal to or greater than 2%
-
United States-born persons who were not vaccinated as infants and whose parents were born in a region of high HBV prevalence (equal to or greater than 8%)
-
Persons with HIV infection
-
Persons with current or past injection drug use
-
Men who have sex with men
-
Infants born to people who are HBsAg-positive
-
Household contact with a person who has HBV infection
-
Needle-sharing or sexual contacts of persons with known HBV infection
-
Patients receiving predialysis, hemodialysis, peritoneal dialysis, or home dialysis
-
Persons with elevated alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels of unclear etiology
-
Persons who request HBV testing due to the potential reluctance to disclose stigmatizing risk factors
-
Additional Clinical Considerations for HBV Screening
The CDC does not provide guidance on the number of sex partners that confer increased risk for HBV acquisition.[5] Medical providers should consider the number of sex partners, type of sexual activity, and timing of prior HBV testing when deciding on repeat testing for people at risk for HBV acquisition.[5] Similarly, there is no clear guidance on the frequency in which HBV testing should be repeated for persons who remain at risk for infection. Decisions regarding the timing and frequency of repeat testing should be individualized based on risk factors, patient age, and immune status.[5]
Rationale for Universal HBV Screening in Adults
Chronic HBV is an indolent and often silent disease that over time can lead to serious health consequences, including cirrhosis, decompensated liver disease, hepatocellular carcinoma (HCC), and death.[6] Universal screening for HBV has the advantage of averting substantial morbidity and mortality and it has been shown to be cost-effective.[7] In addition, universal screening has a number of benefits at the individual and population levels, which are outlined below.[5]
- Chronic HBV infection can be easily detected before the onset of significant liver disease using reliable and inexpensive tests.[5]
- Multiple safe and effective antiviral options are available for persons who have an indication for treatment and can reduce the morbidity and mortality associated with chronic HBV.[4,8]
- Persons identified to have chronic HBV can undergo evaluation for cirrhosis, and if diagnosed with cirrhosis,& can receive further evaluation, management, and prevention of cirrhosis-related complications.[4,8,9]
- Persons with chronic HBV can be evaluated to see if they have an indication for hepatocellular carcinoma surveillance; if indicated, regular surveillance for hepatocellular carcinoma can identify early-stage cancer lesions in the liver that have the potential for cure.[10]
- Persons diagnosed with chronic HBV can receive hepatitis A immunization (if nonimmune) and receive counseling on how to minimize additional liver damage, such as avoiding alcohol intake or excessive acetaminophen ingestion.[3]
- Screening can identify persons who would benefit from hepatitis B vaccination or those who are at risk for HBV reactivation.[5]
- Identifying persons with chronic HBV can reduce the population spread of HBV through treatment of HBV and appropriate treatment and prevention measures.[4]
- Screening of pregnant women can facilitate appropriate management to reduce the risk of perinatal infection.[5]